Denial Management
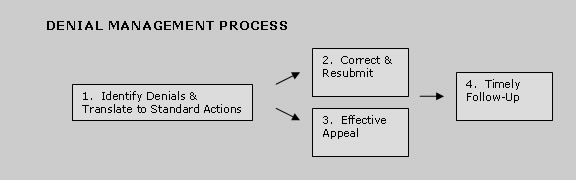
Identify Denial Reason Codes and Correlate to Standard Actions
Every denial has specific reason for non-payment. Once the denial cause is identified, our team will correlate the cause to the appropriate action. For efficiency, actions are standardized and followed accordingly.Correct & Resubmit
For resolving minor errors, a simple correction is all that is needed. The data is corrected and the claim is re-submitted.Sometimes however, correction could involve sending supporting documents, inquiring client for additional information or clarification, and research. All actions are documented as notes in patient accounts for tracking purposes.
Effective Appeals
If the claim is denied despite correct and complete data, we will appeal to the insurance company. We have prepared standard appeal forms for effective response.Timely Follow-up
As receivables get older, there are less chances of getting it collected. Hence we are committed to keep receivables as low as 45 days.Resource planning is done to ensure that all the unpaid claims are being followed up within pre-defined time frame.
- Resource planning is done to ensure that all the unpaid claims are being followed up within pre-defined time frame.
- A Pending Charge reports is generated on a regular basis to identify payments that have not yet been paid.
- EOBs are scrutinized for payments of previous corrections / appeals.
- Insurance companies are contacted to verify receipt of appeals and follow-up.