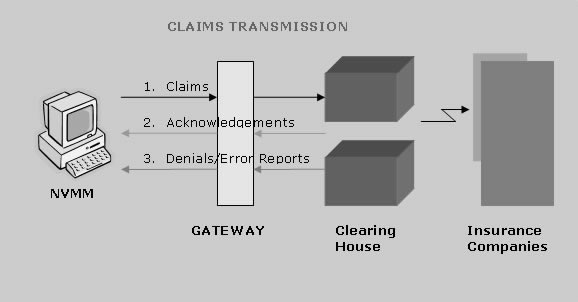
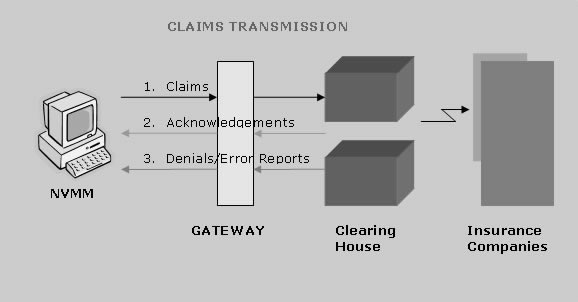
Claim Management Process
Transmit Claims Properly
We will ensure that all the claims are transmitted with all the information as per payer standards. Our team keep themselves updated about any changes by the payer.
Verify Acknowledgements
We keep a track on the acknowledgement report received from both gateway and clearing house for the submitted claims to ensure that there aren’t any claims which are not delivered.
Handle Error / Denial Reports
We will also check and correct any denials or errors encountered from Gateway and Clearing House level. We will resubmit these claims after correction within 24hrs.